In April, the Director of the Maryland Center for Health Equity’s Dr. Stephen B. Thomas (Dr. T), in partnership with FHI Clinical, pulled together a mighty team of experts for a frank conversation about COVID and how to encourage Brown and Black communities to participate in clinical research. The town hall-style discussion included COVID vaccine researchers, health professionals and community activists from across the United States, including FHI Clinical’s own Joy Toro, Claudia Christian and Latrina Watkins. In this post, we summarize what the experts said about where we are in the pandemic, what challenges still lie ahead and what ideas may provide us with solutions.
COVID check-in: Where are we?
…were just a few of the emotions expressed. While it seems things are better, the panelists made clear they feel the pandemic is far from over, and there is much work left to be done. A few panelist comments are summarized here:
Challenges within the health care system
The panel conversation quickly moved to problems Brown and Black communities have when interacting with the health care system and why they have been historically reluctant to participate in clinical research. The FHI Clinical team had a lot to say, as summarized below:
- Navigating a complex health care system
- Lack of treatment alternatives and lack of knowledge to ask about alternatives
- Lack of patient knowledge about how to ask for a second opinion if they feel they need one
- Timing of treatment, transportation, testing requirements and financial obligations
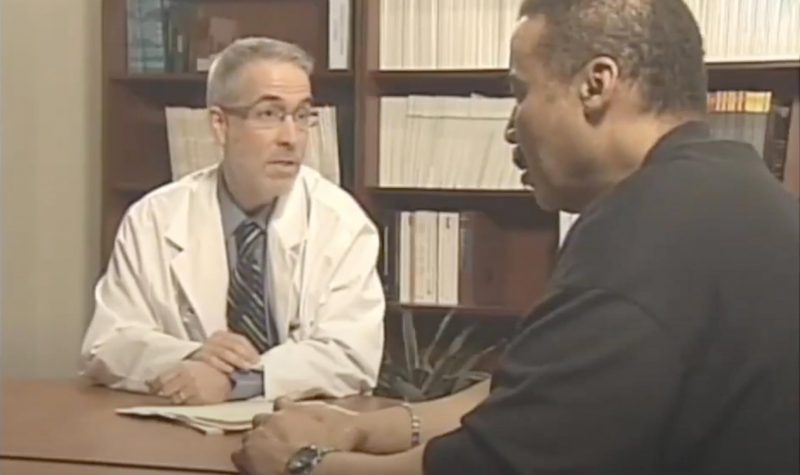
Joy Toro, Senior Director, Clinical Strategy, FHI Clinical: People say we (minorities) don’t want to participate in research, but that’s not really true. People are more inclined to participate after being educated – it just takes a moment to break it down into simple terms. But, we also have to consider the dynamic between the participant, the doctor and the trial. Oftentimes, there are racial undertones or unseen power dynamics. The key is to have cultural sensitivity to those situations. It helps if it’s someone that looks like you giving you the information, but it doesn’t have to be. It comes down to trusting someone you’ve seen in your community. Trust is the foundation.
Sandra Quinn, PhD, Professor and Chair of the Department of Family Science and Senior Associate Director of the Maryland Center for Health Equity, School of Public Health, University of Maryland (UMD): In a national survey, Dr. T and I (with the Maryland Center for Health Equity) asked Latino and African Americans, “What would motivate you to participate in clinical research?” We found that respondents weren’t being asked to participate and that altruism for future generations was a powerful motivator. But, these communities were worried. They don’t trust the system. How can we get health care to be more trustworthy?
Yolanda Ogbolu, PhD, CRNP-Neonatal, FNAP, FAAN, Associate Professor and Chair of the Department of Partnerships, Professional Education, and Practice and former Director of Global Health, University of Maryland (UMD): All the interactions people have had with the health care system have failed them as a human being and led them to mistrust the system. They don’t feel like they can trust providers, so they don’t participate in clinical trials.
Ysabel Duron, Founder, The Latino Cancer Institute (TLCI): Often, there is a language barrier, so patients don’t feel listened to.
Solving the problem: A few ideas
Joy Toro, Senior Director, Clinical Strategy, FHI Clinical: It’s important to have respect for people, and you must get involved in the community. You must also address various barriers to people participating. For example, we have sites that stay open in the evening and on weekends to accommodate more people and do outreach in local languages.
Sandra Quinn, PhD, Professor and Chair of the Department of Family Science and Senior Associate Director of the Maryland Center for Health Equity, School of Public Health, University of Maryland (UMD): We have to train our researchers to have dialogues and have system-wide programs. We can create community research advisory boards. Once we get out there and have conversations with people, the health care system and professionals become less scary, and people feel comfortable asking questions. It’s about building relationships.
As Dr. T points out, COVID presents us with an opportunity to demonstrate cultural sensitivity and awareness and to do a better job at recruiting diverse populations for clinical trials. And while there is still a lot of work to do, things are absolutely changing for the better.

